Three out of four women can develop this genital fungal infection. Here are the answers, delivered by professionals, to know how to identify it and how to prevent it.
If it wasn’t you, it’s very likely that a friend or family member was a victim of candidiasis. An article from Harvard Health Publications details that, throughout their lifetime, 75% of all women are likely to have at least one vaginal Candida infection, and up to 45% experience it two or more times. Candidiasis, as it is generally called candidal vulvovaginitis, This is an infection caused by different Candida-type fungi..
“ There Candida albicans It’s the most common,” explains Alessandra Dulanto, occupational health manager at Pulso Salud. Contrary to what many people believe, this condition does not come from a vaginal infection, but rather from an infection that occurs from the person themselves.
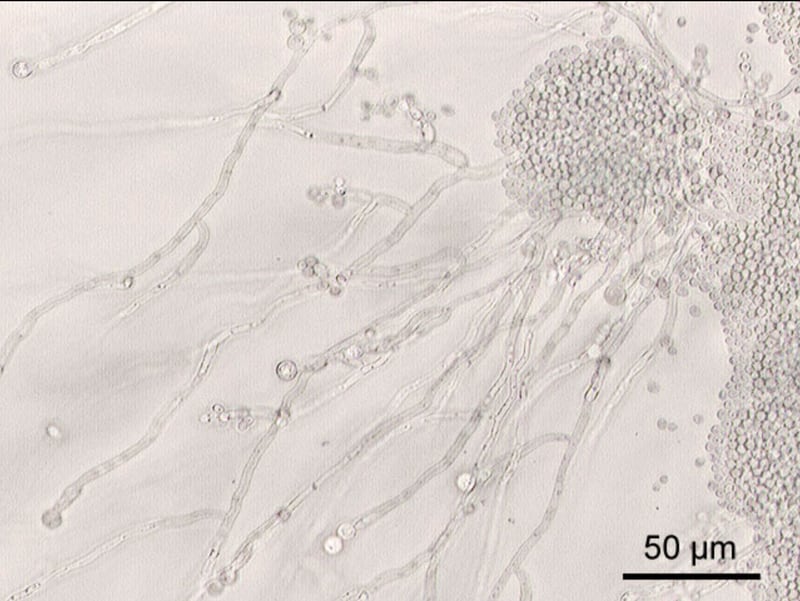
“This fungus usually lives in the vagina and intestine. Although it is present in small amounts, it does not usually cause symptoms,” explains Dulanto. But when women are stressed and their defenses are weakened, whether due to poor diet, lack of sleep, illness, pregnancy or taking antibiotics, they tend to be more likely to contract vaginal candidiasis.
Women with diabetes or immunosuppressive diseases, such as HIV, are also at increased risk. These externalities are ultimately risk factors that “can cause the fungus to grow more than usual,” he says.
Even if we don’t see it, the vaginal microbiota exists and is a fundamental element of our body’s balance. “It is all the micro-organisms, such as bacteria, fungi or even viruses, which naturally inhabit certain parts of the body and do not cause any harm,” explains Sara Parada, director of the obstetrics department at the Andrés Bello University of Santiago.
The big problem with the microbiota is that since we don’t see it, we easily ignore it. “Lactobacilli, for example, are primarily responsible for maintaining and protecting the vaginal ecosystem,” says Parada. This is why it is common for cervicovaginal infections to be the consequence of alterations in the microbiota – whether due to an unbalanced diet, poor hygiene or an episode of stress – which lead to a reduction in immunity. local.
How does this manifest?
In general, Vaginal candidiasis is generally benign and controllable, depending on the treatment indicated by the doctor. However, some women may develop serious infections, involving redness, swelling and cracks in the wall of the vagina.
“Clinical manifestations that women may experience are itching, redness of the genitals, vaginal pain, dyspareunia (pain during sexual activity), dysuria (burning when urinating) and whitish, thick or thin vaginal discharge. sour smell. In more severe cases, cracks or mesh injuries may appear,” says Parada.
Dulanto summarizes the signs like this:
- Erythema: reddish skin
- inflammatory edema : inflammation due to accumulation of fluid in the skin and mucous membranes
- Increased vaginal secretion: sometimes smelly, whitish in color and characteristics, somewhat thick and lumpy. It can also be a bit thick and watery.
The problem, says the Pulso Salud professional, is that “most women cannot know if they have genital candidiasis”, raises Dulanto as a problem, because sometimes the symptoms of the infection are very similar to those of other pathologies.
“The best way to determine if a woman has genital candidiasis is to go see a doctor and, through a vaginal culture, which is the appropriate test to determine the presence of fungus, to see what type of infection it is. “acts,” he explains. .
Treatment of candidiasis
“In general, medical treatment is indicated after clinical evaluation and review of the patient’s medical history. However, the treatment is always local and systemic, although it varies depending on each pathology,” explains Parada.
Vulvovaginal candidiasis, Dulanto supplements, is usually treated with oral tablets, vaginal suppositories and vulvar cream. “Sometimes, pharmacological treatment is not enough to cure an episode, and there are many recommendations to carry out a complete and successful process,” he explains.
A medical approach against candidiasis also generally includes the consumption of probiotics, which will help to improve the diversity of the vaginal microbiota and thus strengthen the defensive system of this area.

“If your condition does not improve after completing treatment, you will need to return to the doctor,” says Dulanto. Sometimes this means repeating the treatment, but in most cases you will need to change medications or strategies. “Generally speaking, there do not seem to be any differences in effectiveness between different treatments, nor between different guidelines,” he comments.
And what about the couple?
Although most vaginal yeast infections are not sexually transmitted, if the partner is male and has symptoms of Candida balanitis — redness, irritation and/or itching of the glans — it may also need treatment.
This is something that should be asked yes or yes during the medical consultation after the diagnosis, because the only way to control the situation, if both people experience it, is jointly. “The couple’s treatment for candidiasis also includes an oral treatment and a topical cream,” adds Dulanto.
How to prevent candidiasis
Anyone who has suffered from a yeast infection knows how unpleasant it is. And for those who have never had it, we sincerely hope that it never affects them, as it is an uncomfortable, painful and very demoralizing infection.
But having it or not having it does not depend on luck. Certain measures can be taken to avoid the bacterial imbalance that causes it. In the following list, Dulanto suggests actions, habits and considerations that will help prevent it.
- Keep your genital area clean and dry : When bathing, avoid soap and rinse only with water.
- Avoid douching: Although many women feel cleaner if they shower after their period or sex, it can actually make vaginal discharge worse. These douches eliminate healthy bacteria that line the vagina and protect it against infections.
- Eat natural yogurt : make sure it contains live cultures of Lactobacillus acidophilus. Otherwise, you can also consume probiotic tablets containing this strain, especially if you are taking antibiotics.
- Use condoms: to avoid getting or spreading other infections during sex.
- Avoid using aerosols: Any feminine hygiene perfume or powder in the genital area can be counterproductive.
- Avoid extremely tight pants : This can cause irritation and excessive sweating, which encourages the appearance of fungus.
- Wear cotton underwear: Synthetic fabrics, as well as silk, can increase sweating and humidity in the genital area, leading to the proliferation of more fungi.
- If you have diabetes : maintain good control of blood sugar levels.
- Avoid wearing wet swimsuits or sportswear for a long time : Change and wash damp or sweaty clothes after each wear.
Source: Latercera
I’m Rose Brown , a journalist and writer with over 10 years of experience in the news industry. I specialize in covering tennis-related news for Athletistic, a leading sports media website. My writing is highly regarded for its quick turnaround and accuracy, as well as my ability to tell compelling stories about the sport.


